ADHD: The Hidden Iceberg Beneath the Surface
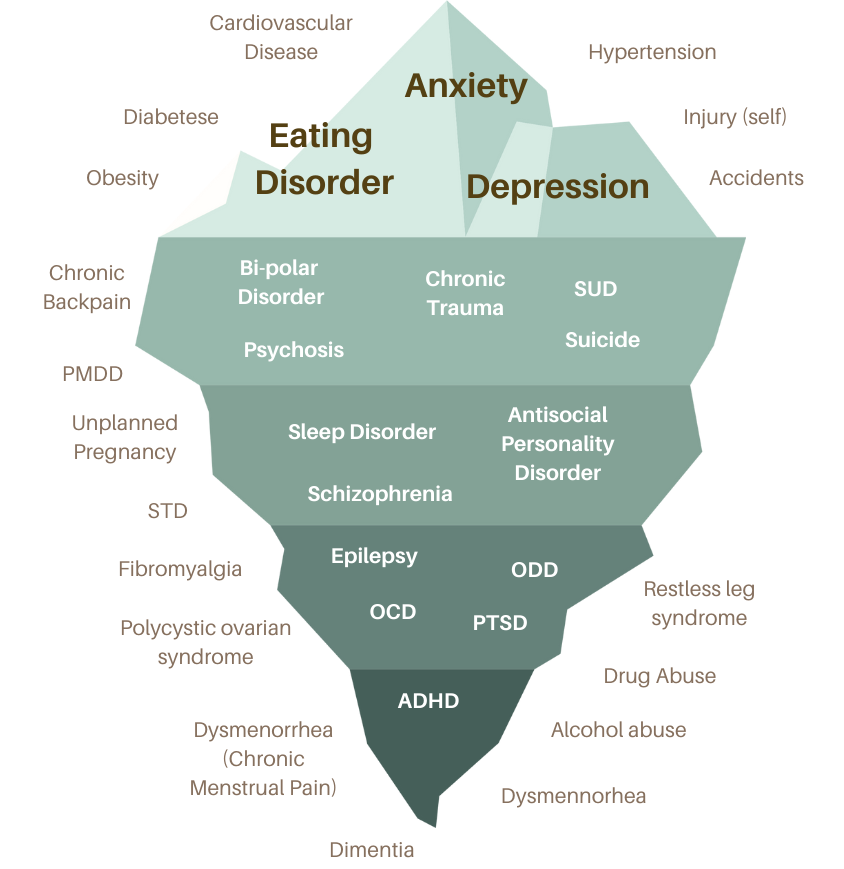
When people think of Attention-Deficit/Hyperactivity Disorder (ADHD), they often picture a hyperactive child who struggles to sit still or an adult who is easily distracted. But ADHD is far more than just trouble focusing—it is deeply interconnected with a range of mental and physical health conditions. The iceberg model in the image below powerfully illustrates how ADHD is just the visible tip of a much larger and more complex web of comorbidities.
The Iceberg Metaphor: What Lies Beneath?
An iceberg floats with only a small portion visible above the water, while most remain submerged. ADHD operates the same way:
- The visible symptoms—impulsivity, inattentiveness, and hyperactivity—are what people commonly associate with the condition.
- However, below the surface lies a deep network of interconnected disorders that often go unnoticed, misdiagnosed, or untreated.
Above the Water: The More Recognized Symptoms
At the top of the iceberg, conditions like anxiety, depression, and eating disorders dominate. These are among the most common co-occurring conditions with ADHD, especially in women.
- Anxiety and Depression: ADHD increases the risk of chronic stress, emotional dysregulation, and low self-esteem, all of which contribute to anxiety and depression.
- Eating Disorders: Impulsivity and executive dysfunction make individuals with ADHD more prone to binge eating disorder (BED), emotional eating, and disordered eating patterns.
Below the Surface: The Deep Comorbidities of ADHD
Mental Health Disorders
The middle section of the iceberg showcases serious mental health conditions that are highly correlated with ADHD:
- Bipolar Disorder & Psychosis: Some individuals with ADHD may experience extreme mood swings and psychotic symptoms, sometimes leading to misdiagnosis.
- Personality Disorders: ADHD’s impact on impulse control, emotional regulation, and social interactions can contribute to the development of antisocial personality disorder or borderline personality disorder traits.
- Schizophrenia & PTSD: Studies show a higher prevalence of schizophrenia and trauma-related disorders in individuals with ADHD. The impulsivity and emotional dysregulation of ADHD can increase susceptibility to traumatic experiences.
Neurological & Cognitive Conditions
Moving deeper into the iceberg, ADHD is closely linked to neurological and cognitive disorders such as:
- Sleep Disorders: Many with ADHD experience chronic sleep disturbances, which further impact focus, mood, and overall health.
- Epilepsy & OCD: ADHD shares genetic and neurological roots with these disorders, making their co-occurrence common.
Hormonal and Physical Health Conditions
At the base of the iceberg, ADHD’s influence extends into women’s health and chronic medical conditions, including:
- Polycystic Ovarian Syndrome (PCOS) & PMDD: Research indicates a higher prevalence of ADHD in women with PCOS and severe premenstrual disorders due to hormonal fluctuations affecting dopamine levels.
- Dysmenorrhea & Fibromyalgia: Chronic pain conditions are often linked to ADHD, possibly due to heightened pain sensitivity and neurotransmitter imbalances.
- Obesity, Diabetes, and Cardiovascular Disease: ADHD’s impact on impulse control, eating habits, and executive function contributes to higher rates of metabolic disorders.
Why Does This Matter?
Understanding ADHD as more than just a focus disorder is crucial for effective diagnosis and treatment. ADHD is a whole-body condition affecting physical, mental, and neurological health.
- Many women with ADHD remain undiagnosed until adulthood, often because their symptoms are masked by anxiety, depression, or hormonal changes.
- Misdiagnosis can lead to inadequate treatment, where the focus is only on surface-level conditions (like anxiety or depression) rather than addressing the underlying ADHD.
- Treating ADHD holistically—through a combination of medication, therapy, lifestyle changes, and hormonal health management—can significantly improve quality of life.
Conclusion: We Need a Deeper Look at ADHD
This iceberg model forces us to rethink ADHD not as an isolated disorder, but as a complex, multi-system condition. If we only treat the symptoms above the water, we fail to address the deeper root causes of suffering for many individuals, particularly women.
The next step? More awareness, more research, and a healthcare system that recognizes ADHD as the foundational condition influencing many others. By taking a whole-person approach, we can ensure that those struggling beneath the surface receive the comprehensive care they need.
Would you like to add specific research citations or a call to action for ADHD awareness?